Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Improve Care in Patients with Pancreatic Pathology
*Corresponding author:Gorecki Gabriel Petre, Titu Maiorescu” University, Faculty of Medicine, CF2 Clinical Hospital, Department of Anesthesia and Intensive Care, Bucharest, 011464, Romania.
Received:April 06, 2023; Published:April 25, 2023
DOI: 10.34297/AJBSR.2023.18.002500
Abstract
The pancreas plays a crucial, fundamental role in the endocrinological control of numerous metabolic processes. The purpose of this study was to find out how to improve care in patients with pancreatic pathology
Through this study we set out to present a number of ways, which can improve care in patients with pancreatic pathology. We also set out to come up with a series of good practices on the medical care side.
Among the ways of improving the care of patients with pancreatic pathology, we find: early detection, multidisciplinary care, minimally invasive procedures, support for support and clinical studies. Regarding the improvement of care in patients with pancreatic pathology, doctors should be aware of risk factors for pancreatic disease, including family history, smoking, obesity and chronic pancreatitis.
Keywords: Pancreas; Pancreatic Pathology; Patient Care; Pancreatic Cancer; Multidisciplinary Care.
Background
The pancreas plays a crucial, fundamental role in the endocrinological control of numerous metabolic processes. Langerhans islands, groups of endocrine cells that produce insulin, glucagon and other hormones in blood flow, play a crucial role in regulating glucose homeostasis [1]. In 2020, about 47,000 cases of worldwide pancreatic cancer were anticipated (Cancer.net). Thus, the sixth most common cause of the deaths caused by global cancer is given by pancreatic cancer. It has also been observed that more developed countries suffer significantly more than the other countries [2].
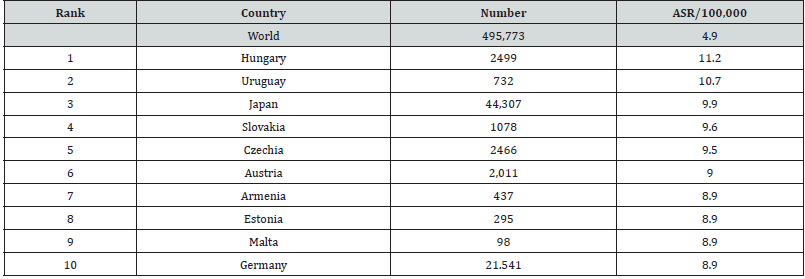
The top 10 countries with pancreatic cancer are Hungary, Uruguay, Japan, Slovakia, Czech Republic, Austria, Armenia, Estonia, Malta and Germany. Pancreatic cancer is still extremely lethal gastrointestinal cancer, in which the survival rate is only 5 years [3]. In 70% of cases, the adenocarcinoma of the pancreatic head manifests itself as painless jaundice caused by the obstruction of the biliary tract together with discomfort, anorexia or weight loss [4]. Rawla’s study (2019) showed that among the causes of pancreatic carcinoma are a number of factors, such as: diabetes, tobacco smoking, dietary factors, age, ethnicity, alcohol abuse, genetic factors, family history and, infection with Helicobacter pylori (Table 1).
Source: World Cancer Research Fund International. Pancreatic cancer statistics. https://www.wcrf.org/cancer-trends/pancreatic- cancer-statistics/
From an etiological point of view, most cases are related to alcohol and smoking abuse [5]. The lack of established, directed screening procedures that can quickly and efficiently identify pancreatic cancer in the early stage in people who are asymptomatic leads to a rather difficult diagnostic process. Regarding the cases that are in the early stage of pancreatic cancer most of the time the recognized symptoms are lacking in the affected persons (Cancer.net).
Improve care in patients with pancreatic pathology
Improving care in patients with pancreatic pathology is particularly important for several reasons: First, pancreatic pathology, which includes pancreatic cancer, pancreatitis and cystic lesions, is associated with a high rate in terms of mortality. In fact, pancreatic cancer has the lowest survival rate of all types of major cancers. By 2030, it is anticipated that pancreatic ductal adenocarcinoma (PDAC), a very aggressive cancer, will occupy the second place in terms of cancer mortality [6]. Which means that improving the care of these patients can contribute to significant results and increased survival rates.
Secondly, patients with pancreatic pathology often have significant symptoms and complications that lead to decreased quality of life. The most common symptoms described by cancer patients, especially those who receive chemotherapy and radiotherapy, are fatigue and discomfort. However, fatigue is in the top, because many patients consider it more annoying than pain [7]. Improving care of these patients can help mitigate symptoms, manage complications and improve general quality of life.
Third, pancreatic pathology is associated with a significant economic burden due to the cost of treatment, hospitalizations and loss of productivity. Hospitalities for acute pancreatitis cost more than $ 2 billion annually, and some demographic categories (people of color and older people) have disproportionately large hospitalization rates [8]. The study of Tingstedt et al. [9] showed that for the remaining life of each patient, the direct cost of treatment was estimated at EUR 16,066 for pancreatic cancer patients. 60% of the total cost of treatment during the treatment was spent on parking. Costs for patients with resectable tumors ranged between 19,809 EUR and 14,899 EUR and 16,179 EUR for patients with metastatic disease. A higher treatment cost than average life has been associated with younger patients and men. Premature mortality represented 79% of productivity loss, which was calculated to be 287,420 EUR for each patient under 65 years old. Improving the care of these patients can help reduce the economic burden of pancreatic pathology on patients, health systems and society as a whole.
Also, improving the care of patients with pancreatic pathology can help accelerate the development and adoption of new treatments and technologies, leading to better results and improving patient care. For example, the study of Singh & O’Reilly [10] showed that pancreatic ductal adenocarcinoma (PDAC) is usually diagnosed at an advanced stage, systemic therapy being the main treatment. The study showed that new therapies appear, and current guides support both germinating and somatic testing in PDAC to evaluate the action. Thus, new therapeutic approaches include strategies for repairing DNA lesions, immunotherapy, stroma and cancer cell metabolism.
Regarding technology, organs represent a technology that develops at a rather alert rate, which contributes to simulating the characteristics on the side of pancreatic tumors [11]. And last but not least, improving the care of patients with pancreatic pathology can have a significant impact on public health by reducing the burden of this disease on families, individuals and society as a whole [12].
Methodology
The purpose of this study is to find out how to improve care in patients with pancreatic pathology. Through this study we intend to present a number of ways, which can improve care in patients with pancreatic pathology. We also intend to come up with a series of recommendations of good practices on the medical care side. So that the providers in the medical field take these, to ensure that the patient receives the best possible care. For this we have selected 7 articles from the last 19 years regarding the assessment of the quality of care provided and to identify the improvement areas. The selection of articles was made from the Google Academic Search Engine. To make the selection of articles we selected the period 2023-2003, in which we were returned 49,500 results for the key pancreatic keyword. Given the large number of articles the selection of articles was made according to their relevance and the number of cities. Finally, they were subjected to the process of analyzing 7 articles from 2004-2019.
In the Analysis Process we Considered the Following Criteria
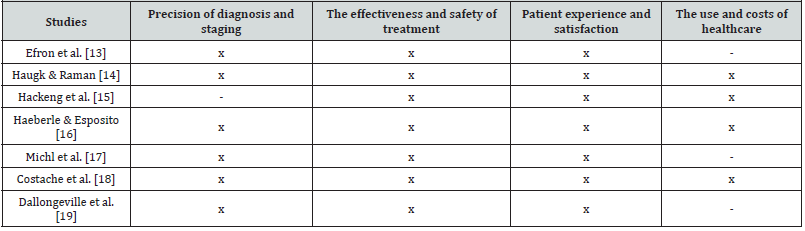
Accuracy of diagnosis and staging. In other words, the accuracy of the diagnosis and the staging is particularly important in terms of determining the appropriate treatment and for predicting the results. Doctors can evaluate the accuracy of the diagnosis and staging by evaluating the use of appropriate imaging and biopsy techniques, as well as the consistency of the stadium results. The efficacy and safety of the treatment through the evaluation of the treatment results, as well as through the survival rates, response, complications, the use of appropriate treatment protocols, including adjuvant therapy and palliative care. The experience and satisfaction of the patient by evaluating the quality of communication and information provided to patients, as well as their access to supporting care services, such as pain management, as well as psychosocial support. The use of medical assistance and the costs associated with the treatment of pancreatic pathology. This contributes to identifying opportunities to improve the efficiency and profitability of providing care.
Result
The study of Efron et al. [13] showed that a safe and effective treatment that preserves the exocrine function and pancreatic endocrine without interfering with the intestinal continuity is central pancreatectomy with pancreaticogastrostomy (Table 2). Regarding the complication of the pancreatic fistula, it was treated conservatively by maintaining surgically implanted drains, and the recovery did not require invasive intervention. The purpose of tissue diagnosis is to identify adenocarcinoma and to differentiate it from non-neoplastic conditions, such as chronic pancreatitis and less frequent and less aggressive pancreatic neoplasms [14]. At the same time, the study showed that the detection of pancreatic lesions using endoscopic biopsy biopsies with ultrasound with ultrasound with incorporated material in paraffin becomes more and more important. When pancreatic tissue samples are examined pathologically, neoplasms can be classified and graded, and the stage information, resection margin and response to neoadjuvant therapy can be obtained in resections. The study of Hackeng et al. [15] showed that we are gradually heading to a time when it will be necessary to combine traditional morphological pathology with genetic characterization to make a more precise diagnosis. Also, the importance of genetic profiling in treatment decisions is increasing. For example, the choice of adapted therapy, such as MTOR inhibitors for pancreatic neuroendocrine tumors or parp inhibitors for malignant diseases with BRCA deficiency. The ideal scenario would be the testing of blood and pancreatic juices for genetic variations that identify patients with a precursor with high risk or an early cancer form. The study of Haeberle & Esposito [16] has shown over time a number of crucial factors for the precise classification of patients. These essential components include a meticulous microscopic examination that takes into account the prognostic significance of elements such as the precise state of the resection (R0 vs. R1 1 mm vs. R1 resection), the histopathological degree of the tumor and the so-called lymph nodes, as well as an examination Very standardized brute of PDAC resection specimens using an axial and ink technique of the circumferential resection (CRM) (LNR). The study of Michl et al. [17] showed that when a patient has symptoms that could indicate pancreatic cancer, ultrasonography is usually the first imaging technique. It is easily accessible, safe and offers most patients a quick pancreas examination. It has a good sensitivity to determine the degree of blockage and dilation of the biliary tract. For tumors greater than 3 cm, the sensitivity of ultrasound to identify pancreatic cancer is 95%, but it decreases dramatically with smaller tumors.
Costache’s et al. [18] showed that the most common imaging techniques for diagnosing and staging pancreatic cancer are computed tomography, magnetic resonance imaging and endoscopic ultrasonography. CT showed a diagnostic accuracy of 83.3%, with sensitivity and specificity of 81.4%and 43%respectively. The MRI showed a higher diagnostic accuracy compared to CT (89.1%). However, EUS demonstrated the best diagnostic value in PC (92.7%accuracy).
The study of Dallongeville et al. [19] showed that the best imaging technique for diagnosing and staging pancreatic cancer is computerized tomography (CT). Because their involvement can prevent surgical resection or involve an neoadjuvant strategy in locally or venous -advanced resecable tumors, essential arterial and venous structures are particularly important to be identified with CT. When it comes to isodensic tumors or the existence of tiny liver metastases, MRI provides additional staging information that a scan CT cannot. The reference method for obtaining histological evidence is endoscopic ultrasonography.
Discussions
There are a number of ways to improve the care of patients with pancreatic pathology, including: early detection, multidisciplinary care, minimally invasive procedures, support and clinical studies Early detection of pancreatic pathology is crucial to improve the patient’s results. Early detection initiatives should focus on people with high risk of pancreatic cancer, such as those with family history, newly diagnosed diabetes or precancerous pancreatic cysts due to low pancreatic cancer in the general population [20]. Also, the time between the diagnosis of chronic pancreatitis and pancreatic cancer is often one to two decades; Pancreatitis develops frequently one or two before the discovery of pancreatic cancer as a result of the ductal blocking caused by tumors [21]. However, identifying people at risk of the general population who would benefit from longitudinal surveillance programs, as well as the use of appropriate biomarkers and imaging modalities for the supervision of pancreatic ductal adenocarcinoma, are obstacles for early detection [22].
In terms of multidisciplinary care, fewer patients receive only one type of therapy, because the care of pancreatic cancer patients has become more sophisticated. Currently, chemotherapy, radiotherapy and/or surgery are used to treat most patients with such cancer [23]. In addition, to promote a reduced variation in practice patterns, to ensure the proper use of healthcare resources, to provide educational opportunities for medical professionals and to improve the results of cancer care for certain patient populations, multidisciplinary councils for tumors. are frequently used to coordinate care [24]. On the side of minimally invasive procedures, pancreatic neuroendocrine tumors and precancerous pancreatic cystic lesions can be treated minimally invasive and possibly permanent using endoscopic ablation with ultrasound -guided radiofrequency [25].
Without endoscopic ultrasound, it would simply be impossible to diagnose pancreatic and biliary neoplasms due to variety and extension of its therapeutic uses. Endoscopic ultrasound has been shown to be an incontestable diagnostic tool, and now therapeutic applications have an improvement in potential and safety. Important choices regarding the preservation or sampling of organs or the execution or non -performance of endoscopic resection can be done thanks to the endoscopic ultrasound, especially when the involvement of the lymph nodes can be proved by imaging [26].
Thus, the standard for the evaluation of the pancreaticobiliary tree continues to be endoscopic retrograde cholangiopancreatography. The risk of serious consequences is the main disadvantage of this invasive procedure. Pancreatitis and cholangitis, which occur in 5.4% and 1.0% of patients with biliary sphincterotomy, are the most common significant and potentially fatal consequences of endoscopic retrograde cholangiopancreatography [27].
The use of minimally invasive surgical techniques for pancreatic diseases has increased as a result of progress in science and technology, such as laparoscopic surgery. Laparoscopic laparoscopic pancreaticiactomy (LPPPD), left pancreatic resection, laparoscopic distal pancreatectomy (LDP) and laparoscopic surgery for island cell tumor were the first minimally invasive pancreatic procedures for neuroendocrine tumors of the pancreas, laparoscopic methods [28].
The multidisciplinary approach to chronic pain management should include behavioral therapies, especially when the psychological impact [29]. Treatment of pancreatic pain in the context of the patient with complex chronic visceral pain, with physical, psychological and psychosocial conditions, is still a challenge [30]. In addition, O’Reilly et al and to facilitate the improvement of the result. Thus, the diagnosis, stage, hereditary monitoring with high risk, psychological support, pain treatment, nutrition management and special management with resectable pancreatic cancer, resecable and non -removable were recommended [31-33].
Conclusions and Recommendations
Regarding the improvement of care in patients with pancreatic pathology, doctors should be aware of risk factors for pancreatic disease, including family history, smoking, obesity and chronic pancreatitis. Patients with high risk of pancreatic disease should undergo periodic controls, including imaging tests and blood tests.
Sleep apnea
The healthcare issues in neurological patients can also lead to the development of obstructive sleep apnea [131]. Obstructive sleep apnea (OSA) is a complex disease related to the dysregulation of the molecular clock and other associated biological processes [132]. The hypothesis being put forth in OSA is that the monoaminergic neurons (noradrenergic and serontonergic) inhibit cholinergic neurons leading to suppression of REM sleep and upregulating NREM sleep. This is due to the decrease in firing frequency of monoaminergic neurons in NREM sleep, and increase in firing of cholinergic neurons in REM sleep. The process leads to the development of a recurring cycle [133]. Sleep apnea is associated with many other complications including Down’s syndrome [134]. Understanding molecular biology of sleep apnea can lead to the development of new treatments [135]. There are a few reports that have shown the molecular domains affected in OSA, adipokines, celladhesion molecules and molecules responding to the endoplasmic reticulum stress [136].
The management of pancreatic pathology often requires a multidisciplinary approach, which involves gastroenterologists, oncologists, radiologists and surgeons. The collaboration between these specialists can help ensure that patients benefit from complete and coordinated care. Minimally invasive procedures, such as endoscopic ultrasound and laparoscopic surgery, can be used to diagnose and treat pancreatic pathology. These procedures are associated with fewer complications, shorter hospitalizations and faster recovery times compared to traditional open surgery.
We also intend to offer a series of recommendations of good practices on the medical care side. Thus, providers in the medical field must take into account a number of several aspects to ensure that the patient receives the best possible care.
In addition, patients with pancreatic pathology may require supporting care to manage symptoms and improve their quality of life. This may include pain management, nutritional support, but also psychological support.
A first recommendation is about the patient’s safety. Medical service providers must ensure that the patient is safe and that he will not suffer injury or injury during care period. Thus, it must be ensured that the patient will be fixed correctly on the examination table or in the wheelchair. Also, medical providers must ensure that all medical equipment is used in a correct way, under the safest conditions, and the patient does not receive wrong medicines.
The second recommendation is about respecting confidentiality. Thus, patients are entitled to the confidentiality of their medical information, and their medical information should not be revealed to other people without their consent. Another recommendation is to respect the patient’s legal and moral rights regarding their medical care. At the same time, the rights of patients in information must be respected and participating in the decision -making process. Another recommendation is to ensure effective communication with the patient to understand his health problems and to explain the treatment options. Also, medical staff should listen to the patient’s concerns and questions and answer them clearly and honestly.
And last but not least, another recommendation is due to compliance with medical norms and protocols, including those related to hands hygiene, sterilization of medical equipment and correct drug administration.
Therefore, by going through the best care practices, a safe and efficient medical experience will be ensured.
The limits of this study consist of the small number of articles that have been subjected to analysis, which means that the data cannot be generalized.
Declaration of Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests.
References
- Whitley EM (2014) Comparative Pancreatic Pathology. Pathobiology of Human Disease pp. 1101-1123.
- Rawla P (2019) Epidemiology of prostate cancer. World J Oncol 10(2): 63.
- Hu JX, Zhao CF, Chen WB, Liu QC, Li QW, et al. (2021) Pancreatic cancer: A review of epidemiology, trend, and risk factors. World journal of gastroenterology 27(27): 4298-4321.
- Bellizzi AM, Frankel WL (2009) Pancreatic pathology: a practical review. Lab Med 40(7): 417-426.
- Klöppel G (2007) Chronic pancreatitis, pseudotumors and other tumor-like lesions. Modern pathology 20(Suppl 1): S113-S131.
- D'Onofrio M, Zamboni G, Malagò R, Martone E, Falconi M, et al. (2005) Pancreatic pathology. Contrast Media in Ultrasonography: Basic Principles and Clinical Applications pp. 335-347.
- Yeo TP, Burrell SA, Sauter PK, Kennedy EP, Lavu H, et al. (2012) A progressive postresection walking program significantly improves fatigue and health-related quality of life in pancreas and periampullary cancer patients. Journal of the American College of Surgeons 214(4): 463-475.
- Fagenholz PJ, Ferna C, Harris NS, Pelletier AJ, Camargo Jr CA (2007) Direct medical costs of acute pancreatitis hospitalizations in the United States. Pancreas 35(4): 302-307.
- Tingstedt B, Andersson E, Flink A, Bolin K, Lindgren B, et al. (2011) Pancreatic cancer, healthcare cost, and loss of productivity: a register-based approach. World journal of surgery, 35(10): 2298-2305.
- Singh RR, O’Reilly EM (2020) New treatment strategies for metastatic pancreatic ductal adenocarcinoma. Drugs 80(7): 647-669.
- Chen H, Zhuo Q, Ye Z, Xu X, Ji S (2021) Organoid model: A new hope for pancreatic cancer treatment?. Biochim Biophys Acta 1875(1): 188466.
- Huang J, Lok V, Ngai CH, Zhang L, Yuan J, et al. (2021) Worldwide burden of, risk factors for, and trends in pancreatic cancer. Gastroenterology 160(3): 744-754.
- Efron DT, Lillemoe KD, Cameron JL, Yeo CJ (2004) Central pancreatectomy with pancreaticogastrostomy for benign pancreatic pathology. J. Gastrointest Surg 8(5): 532-538.
- Haugk B, Raman S (2016) Pancreatic pathology: an update. Surgery (Oxford) 34(6): 273-281.
- Hackeng WM, Hruban RH, Offerhaus GJA, Brosens LA (2016) Surgical and molecular pathology of pancreatic neoplasms. Diagn Pathol 11(1): 47.
- Haeberle L, Esposito I (2019) Pathology of pancreatic cancer. Transl. Gastroenterol. Hepatol 4: 50.
- Michl P, Pauls S, Gress TM (2006) Evidence-based diagnosis and staging of pancreatic cancer. Best practice & research Clinical gastroenterology 20(2): 227-251.
- Costache MI, Costache CA, Dumitrescu CI, Tica AA, Popescu M, Baluta EA, et al. (2017) Which is the best imaging method in pancreatic adenocarcinoma diagnosis and staging-CT, MRI or EUS?. Curr. Health Sci J 43(2): 132-136.
- Dallongeville A, Corno L, Silvera S, Boulay Coletta I, Zins M (2019) Initial diagnosis and staging of pancreatic cancer including main differentials. In Seminars in Ultrasound, CT and MRI 40(6): 436-468.
- Pereira SP, Oldfield L, Ney A, Hart PA, Keane MG, et al. (2020) Early detection of pancreatic cancer. The lancet Gastroenterology & hepatology 5(7): 698-710.
- Raimondi S, Lowenfels AB, Morselli-Labate AM, Maisonneuve P, Pezzilli R (2010) Pancreatic cancer in chronic pancreatitis; aetiology, incidence, and early detection. Best practice & research Clinical gastroenterology 24(3): 349-358.
- Singhi AD, Koay EJ, Chari ST, Maitra A (2019) Early detection of pancreatic cancer: opportunities and challenges. Gastroenterology 156(7): 2024-2040.
- Pawlik TM, Laheru D, Hruban RH, Coleman J, Wolfgang C L, et al. (2008) Evaluating the impact of a single-day multidisciplinary clinic on the management of pancreatic cancer. Annals of surgical oncology, 15(8): 2081-2088.
- Brauer DG, Strand MS, Sanford DE, Kushnir VM, Lim KH, et al. (2017) Utility of a multidisciplinary tumor board in the management of pancreatic and upper gastrointestinal diseases: an observational study. Hpb 19(2): 133-139.
- Karaisz FG, Elkelany OO, Davies B, Lozanski G, Krishna SG (2023) A Review on Endoscopic Ultrasound-Guided Radiofrequency Ablation (EUS-RFA) of Pancreatic Lesions. Diagnostics 13(3): 536.
- Prager M, Prager E, Sebesta Jr C, Sebesta C (2022) Diagnostic and Therapeutic Indications for Endoscopic Ultrasound (EUS) in Patients with Pancreatic and Biliary Disease—Novel Interventional Procedures. Current Oncology 29(9): 6211-6225.
- Scheiman JM, Carlos RC, Barnett JL, Elta GH, Nostrant TT, et al. (2001) Can endoscopic ultrasound or magnetic resonance cholangiopancreatography replace ERCP in patients with suspected biliary disease? A prospective trial and cost analysis. The American journal of gastroenterology 96(10): 2900-2904.
- Shirota T, Nagakawa Y, Sahara Y, Takishita C, Hijikata Y, et al. (2018) Surgical resection of neuroendocrine tumors of the pancreas (pNETs) by minimally invasive surgery: the laparoscopic approach. Gland Surgery 7(1): 12-19.
- Drewes AM, Bouwense SA, Campbell CM, Ceyhan GO, Delhaye M, et al. (2017) Guidelines for the understanding and management of pain in chronic pancreatitis. Pancreatology, 17(5): 720-731.
- Morgan K, Owczarski SM, Borckardt J, Madan A, Nishimura M, et al. (2012) Pain control and quality of life after pancreatectomy with islet autotransplantation for chronic pancreatitis. Journal of Gastrointestinal Surgery, 16(1): 129-133.
- O'reilly D, Fou L, Hasler E, Hawkins J, O'connell S, et al. (2018) Diagnosis and management of pancreatic cancer in adults: A summary of guidelines from the UK National Institute for Health and Care Excellence. Pancreatology 18(8): 962-970.
- Pancreatic cancer statistics. WCRF International.
- (2019) Pancreatic Cancer – Statistics.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.